Cervical Screening Test
You are eligible for a Cervical Screening Test if you are aged between 25 and 74, sexually active (or ever have been) and a woman or person with a cervix.

The cervical screening test (CST) is a new, more accurate way of protecting cervix owners against cervical cancer. It was introduced in Australia in December 2017, and is expected to protect almost one third more people from cervical cancer than the old Pap test.
The Pap test used to look for changes in the cells of the cervix, the entrance to the uterus (womb) from the vagina. Now the cervical screening test looks for evidence of the human papillomavirus (HPV), which can lead to cell changes in the cervix, if left untreated.
If you are a cervix owner aged 25 to 74, you should have your first cervical screening test 2 years after your last Pap test. A common concern among young people is the new age range for cervical screening as previously cervical screening started at age 18. Research shows us that having a five-yearly Cervical Screening Test from the age of 25 is safer and more effective than having a two-yearly Pap test from the age of 18.
The cervical screening test looks and feels the same as the Pap test. But it is only done every 5 years instead of every 2 years, if your results are normal. Research has shown that having a Cervical Screening Test every five years is more effective than, and just as safe as, a Pap test every two years. The renewed program is expected to reduce cervical cancer rates and deaths by at least another 20%.
Cervical cancer is extremely rare under the age of 25 – there are around 10–15 cases of cervical cancer in people under 25 in Australia each year from a total number of around 900 cases.
Since the HPV Vaccination Program was introduced in 2007, the number of cervical abnormalities among people with a cervix aged younger than 25 has been dropping, resulting in fewer cases of cervical cancer in this age group. The combined approach of the vaccine and a more effective cervical screening program is protecting young generations from the risk of cervical cancer.
Self collection
All cervical screening participants now have the choice to self-collect their own Cervical Screening Test sample. A self-collected sample is taken from the vagina and is checked for human papillomavirus (HPV) – a common infection that causes almost all cervical cancers.
If you are eligible and want to collect your own sample, your healthcare provider will give you a swab and instructions.
A self-collected sample is taken from the vagina so you don’t need to worry about reaching the cervix or ‘getting the right spot’. All you need to do is insert a swab a few centimetres into your vagina and rotate it for 20 to 30 seconds.
You will be given a private space (bathroom) to collect your sample.
I have my result. Now what?
This handy flow chart can help you understand your next appropriate follow up
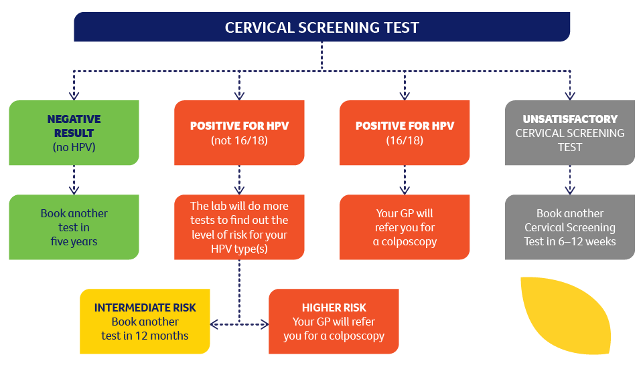
If your Cervical Screening Test shows that you have tested positive for HPV types that need further investigation or that you have abnormal cells that may need treatment, you will be referred to a gynaecologist for a colposcopy. This does not mean that you have cervical cancer.
A colposcopy is a procedure that feels like having a Cervical Screening Test and involves the specialist looking at the cells of the cervix more closely. A colposcopy generally takes 10 to 15 minutes and the doctor may decide to take a sample of tissue (a biopsy) from the cervix for further testing.
LGBTQI+
LGBTQI people aged between 25 and 74 with a cervix need regular cervical screening, because no matter who you have had as a sexual partner or what your gender identity is, you're still at risk of cervical cancer.
Almost all cervical cancers are caused by human papillomavirus (HPV). The virus is passed on by intimate genital skin-to-skin contact, and it is not passed on by semen, blood or saliva.
Choosing a health professional you are comfortable with is important, as they should use language that acknowledges diversity. The Bubble Launceston welcomes and respects diversity of all forms. We understand the barriers LGBTQI people with a cervix may face when seeking cervical screening and appreciate it may be challenging.
The choice to disclose information about your sexuality and gender identity is yours. However, disclosing this personal information may lead to a better experience because your doctor will be able to tailor your care based on how you identify.
If you choose to disclose, let your doctor know whether or not you want it recorded, as other professionals could have access to your medical records. Health professionals are required by law to protect your confidentiality and maintain your privacy.
When you have your cervical screening appointment, you may be asked questions such as 'Are you sexually active?' and 'What form of contraception are you using?'. These questions and assumptions can be uncomfortable, so it's a good idea to think about how you would like to respond beforehand.









